Professor Yamei Tang’s team Achieved Important Progress in Precise Treatment in Brain Necrosis after Radiotherapy
On July 29, 2020, Professor Yamei Tang’s team published an article named “A Radiomics Model for Predicting the Response to Bevacizumab in Brain Necrosis after Radiotherapy” online in Clinical Cancer Research (2019 IF: 10.107). Professor Yamei Tang is the corresponding author. Jinhua Cai et al. are the co-first authors.
Radiotherapy is a key component in the management of head and neck tumors, which may cause different degree of damage and lead to brain necrosis in 3%–24% of patients. Currently, corticosteroid therapy is used for brain necrosis, but with various side effects, and only 35% of patients may get benefit. Bevacizumab, a humanized monoclonal antibody against VEGF, has been shown to decrease the volumes of necrosis by 52%–64%, and the effective response rate is approximately 66%. However, some patients failed to derive adequate benefit from bevacizumab or even worsened, and some may suffer from severe adverse events. Therefore, there is a great need to differentiate patients who are likely to have a good response to bevacizumab from those who are not, so as to provide more personalized targeted therapy and free patients who might have a poor treatment response from risk of those severe side effects.
Radiomics involves high-throughput extraction of large amounts of image-based features from standard medical radiographic images and determination of the relationships between such features and potential pathophysiology. Radiomics is now gaining importance in cancer research because of its potential to aid in diagnosis, evaluation of prognosis, and prediction of response to treatment in a non-invasive manner.
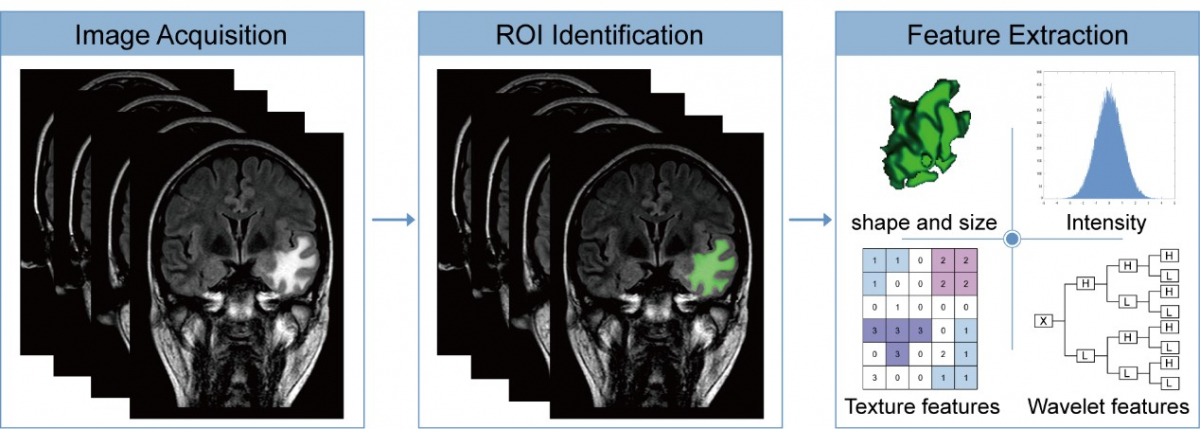
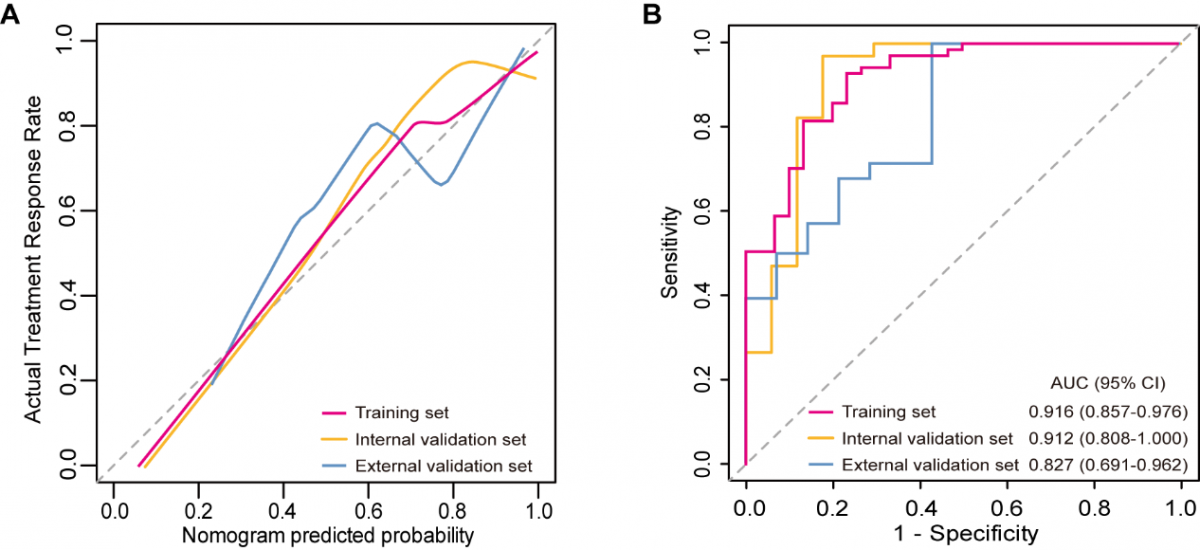
In this study, we developed a radiomics model that integrates a radiomics signature originating from pre-treatment MRI and clinical variables for individualized prediction of the response to bevacizumab in patients with brain necrosis. In the training set, the calibration curve of the radiomics model estimating the probability of an effective treatment response demonstrated good agreement, and an AUC of 0.916 (95% CI, 0.857–0.976) indicated that the model had good discrimination. The favorable performance of the model was validated in the internal and external validation sets, with AUCs of 0.912 (95% CI 0.808–1.000) and 0.827 (95% CI 0.691–0.962), respectively. The presented radiomics model, available as an online calculator, can serve as a user-friendly tool for individualized prediction of the response to bevacizumab in patients with brain necrosis after radiotherapy. This may provide an illustrative example of precision medicine and affect treatment strategies.
This work was supported by the National Key R&D Program of China (2017YFC1307500, 2017YFC1307504), the National Natural Science Foundation of China (81925031, 81820108026), and the Science and Technology Program of Guangzhou (202007030001) to Yamei Tang.
Article link: https://clincancerres.aacrjournals.org/content/early/2020/09/01/1078-0432.CCR-20-1264.long


